The emergence and ongoing advancement of clinical artificial intelligence (AI) have been revolutionary. Initially viewed as experimental, the technology is now proving its worth in esteemed institutions worldwide, delivering unforeseen benefits in its early stages of development. Beyond simply flagging potential positive findings and prioritizing radiologist worklists, AI’s impact is now extending beyond the workstation, influencing patient care pathways in critical service areas like cardiovascular and neurology. While the adoption of AI brings numerous advantages for physician workflows, there is one aspect that clinicians are not as enthusiastic about: alert fatigue. This phenomenon must be avoided, particularly in scenarios such as PERT activations.
What is Alert Fatigue?
Similar to the moral of Aesop’s fable “The Boy Who Cried Wolf,” alert fatigue refers to the excessive notifications specialists receive regarding a specific condition, especially when a case does not require their immediate attention. This can lead to a lack of seriousness in specialists’ interpretations when bombarded with AI notifications on their mobile devices.
Let’s consider this in the context of pulmonary embolism (PE) cases.
Avoiding Alert Fatigue & Unnecessary PERT Activations
The role of AI in pulmonary embolism cases is crucial. As one of the leading causes of death from cardiovascular disease, PE is often referred to as the “silent killer” due to its high mortality rate when left untreated. This highlights the importance of promptly notifying a facility’s pulmonary embolism response team (PERT) about potential PE cases. AI plays a significant role in this process, as not all PE cases require the same level of intervention from the interventionalist.
There are different grades of severity for PE cases:
- Massive – Severe obstruction of the pulmonary arterial tree causing acute cardiopulmonary failure, requiring immediate specialist intervention and PERT consultation.
- Sub-Massive – Acute PE with myocardial necrosis, often treated with anticoagulants unless RV dysfunction is present. PERT consultations are less common in these cases.
- Non-massive – Stable PE with normal RV function, typically managed with anticoagulant therapy and not requiring PERT consultation.
Considering the potential for alert fatigue, it is evident that not every PE case warrants a PERT activation, as this can lead to diminishing value of AI notifications with each unnecessary consultation.
To offset PE alert fatigue in a facility, AI must:
- Implement additional risk stratification measures, such as the ability to assess the RV/LV ratio.
- Use this information to evaluate the severity of the PE and notify the PERT only when specific criteria are met.
- Integrate with electronic health records (EHR) to provide real-time lab values for accurate triaging and timely PERT consultations.
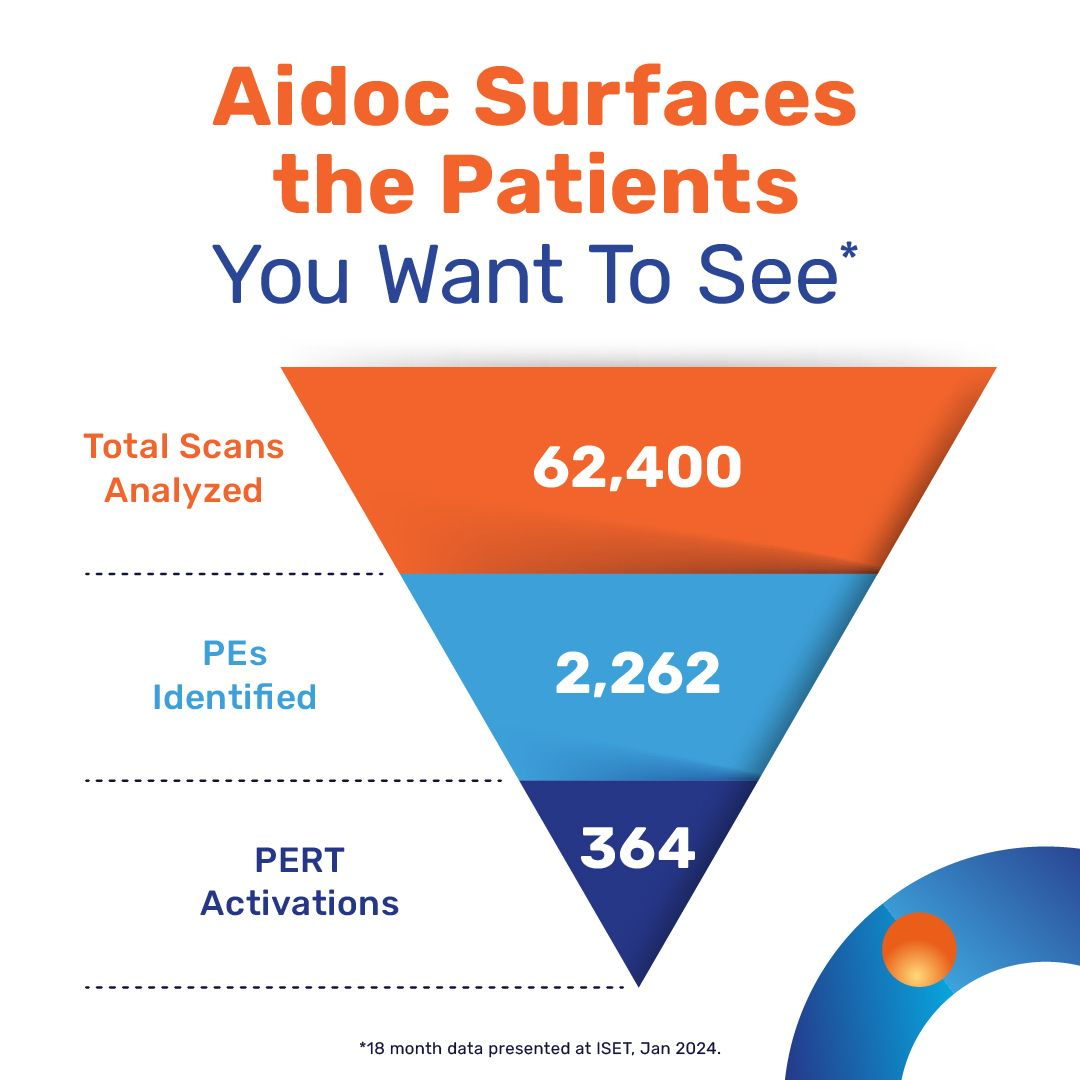
The graphic below illustrates how AI can significantly reduce unnecessary PERT activations over an 18-month period, focusing on patients who truly require consultation.
Ending the Fatigue
Without AI incorporating additional risk stratification measures, clinicians may experience alert fatigue, where each notification carries less weight than the previous one. An AI workflow lacking this layer of sophistication can not only cause inconvenience but also impact a patient’s treatment plan.
For a new technology to truly excel in this field, it must be effective, user-friendly, and widely adopted. In cases like PE, timely treatment decisions can significantly impact patient outcomes. AI must be able to trigger PERT activations at the right moment, with parameters in place to prevent alert fatigue, ensuring that specialists trust the importance of every PE notification and give it the attention it deserves.